
Scaling up naloxone access to save lives
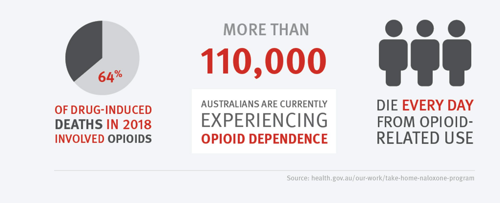
Burnet Institute welcomes and supports the national rollout of Take Home Naloxone (THN) in Australia – and the challenge to ensure access to this life-saving medicine for people at risk of opioid overdose or an adverse reaction.
Administered by injection or nasal spray, naloxone is a safe, reliable and effective medication that can temporarily reverse the effects of overdose from opioid drugs such as heroin or oxycodone.
THN programs involve training and naloxone dispensing so it can be administered by carers, friends or family members of the person experiencing an overdose, who may be unconscious, or unable to breathe effectively.
See also: What is naloxone and how can it help save drug users who overdose?
Since 1 July 2022, naloxone has been available free of charge without prescription through the Australian Government’s Take Home Naloxone s100 special access program, from pharmacies and from other dispensing points.
“It’s really amazing and a huge step forward to have this life-saving medicine freely available through Australian Government funding,”
Professor Paul Dietze, Co-Program Director, Disease Elimination, Burnet Institute
“The task now is to ensure that we get it to people who are most at risk.”
Those most at risk essentially comprise two groups – people who inject drugs, and people who take opioids for other reasons, such as chronic pain.
“The people who are injecting drugs may have an understanding or an experience with overdosing, so to provide them with an overdose antidote to use on people they might come across makes sense for them,” Professor Paul Dietze said.
“But there’s not that same experience or awareness among people taking opioids for chronic pain who don’t appreciate that opioid drugs carry a risk of overdose.
“So, educating them, and educating pharmacists in particular about the availability of naloxone and how to use it is still a major requirement to reach all people who can benefit from naloxone.”

Fully capitalising on Australian Government funding will take a collective effort, including research on models that work in different settings, and support from peak bodies such as the Pharmacy Guild and Pharmaceutical Society of Australia, the College of General Practitioners, and drug treatment and consumer organisations.
“General practitioners and pain specialists also have roles to play, along with harm reduction workers based at needle and syringe programs, for example, who are well equipped to do this work,” Professor Dietze said.
“I’m sure they can use extra support, but they’ve already got mechanisms in place to have an impact.”
While the Australian Government provides the funding, the implementation of THN programs rests primarily with Australia’s states and territories, where regulatory requirements vary in approach and effectiveness.
In Western Australia, for example, many police now routinely carry naloxone in the event they encounter someone who’s overdosed, while New South Wales is leading the way with their naloxone program operating in the state’s prison system.
“Working to ensure that naloxone gets to people who are at risk in WA includes working with police and paramedics,” Professor Dietze said.
“In Victoria, we’re not doing that yet, and that’s something that we should be exploring.
“Mechanisms of engaging with the people who need it, that’s the fundamental thing.”
See also: Time to explore decriminalisation of drug use on International Overdose Awareness Day
Professor Dietze said the National Naloxone Reference Group, convened by Burnet Institute, has been important for key stakeholders involved in jurisdictional naloxone programs to share information and learnings, and strategise for expanding THN in Australia.
The Burnet-led EC Australia partnership to eliminate hepatitis C in Australia by 2030 may also be an effective model for what can be achieved with THN.
“Much like EC Australia, it’s about implementation science to make sure that we work out the best ways to get more naloxone into the hands of the people who need it.”
“There’s a lot of work that can be done around implementation,” Professor Dietze said.
Internationally, Australia stands to benefit from work undertaken by the World Health Organization and United Nations Office on Drugs and Crime, and there are learnings to be had from programs in other countries who face similar challenges to ours.
“In Canada they’ve had very extensive programs to get naloxone to the target populations, and in the United States they’ve had extensive work going on there as well,” Professor Dietze said.
“But the cost of naloxone in some of those places is prohibitively high and so the Australian Government funding of intranasal naloxone in particular, to make it available free of charge is a real game changer in the Australian context.
“We’re extremely fortunate, and we need to make the most of this great opportunity.”
You're reading IMPACT magazine | Subscribe today
More stories of IMPACT
- VOICE: Building on pandemic lessons and community strengths
-
How Burnet’s Papua New Guinea team has responded to the challenges of COVID-19
-
On the road to 2030: breaking down the entrenched barrier to hepatitis C elimination
-
A visit to Burnet starts a family’s 35-year relationship with the Institute
-
Building confidence and dispelling stigma around sexual and reproductive health
Make an Impact - Donate Today
Please donate today and support healthy mothers, children and adolescents. Every donation makes a difference to the lives of vulnerable communities.




